Thyroid Cancer
Abstract
Thyroid cancer is the most common endocrine tumor. Thyroidectomy, radioactive iodine, and TSH suppression represent the standard treatment for differentiated thyroid cancer. Since chemotherapy has been shown to be unsuccessful in case of advanced thyroid carcinomas, the research for new therapies is fundamental. Studies of many tyrosine kinase inhibitors as well as antiangiogenic inhibitors suggest that patients with thyroid cancer could have an advantage with new target therapy. We summarized both the results obtained and the toxic effects associated with these treatments reported in clinical trials. Reported data are encouraging, but further trials are necessary to obtain a more effective result in thyroid carcinoma treatment.
1. Introduction
Thyroid cancer is rare, but is the most prevalent endocrine malignancy tumor. In 2002, in the USA 141,000 cases occurred and 35,300 deaths were estimated Among different parts of the world there is a 10-fold difference in incidence for women, but only a 3-fold difference for men .
The differences between the sexes declines after the middle age, but still three out of four cases arise in women. The most well-established cause of thyroid cancer is the exposure to ionizing radiations, particularly during childhood. Iodine deficiency influences thyroid function directly as well as indirectly, through a reduction of thyroid hormones levels and a consequent increase in TSH secretion. Chronic iodine deficiency is firmly established as a risk factor for goiter and follicular thyroid cancer, while some aetiological studies suggested that iodine supplementation programmes could increase the incidence of papillary thyroid cancer by inducing iodine excess. Supplementation effects are likely to be confused by diagnostic procedures improvement and therefore there may be not a biological background at the basis of this phenomenon .
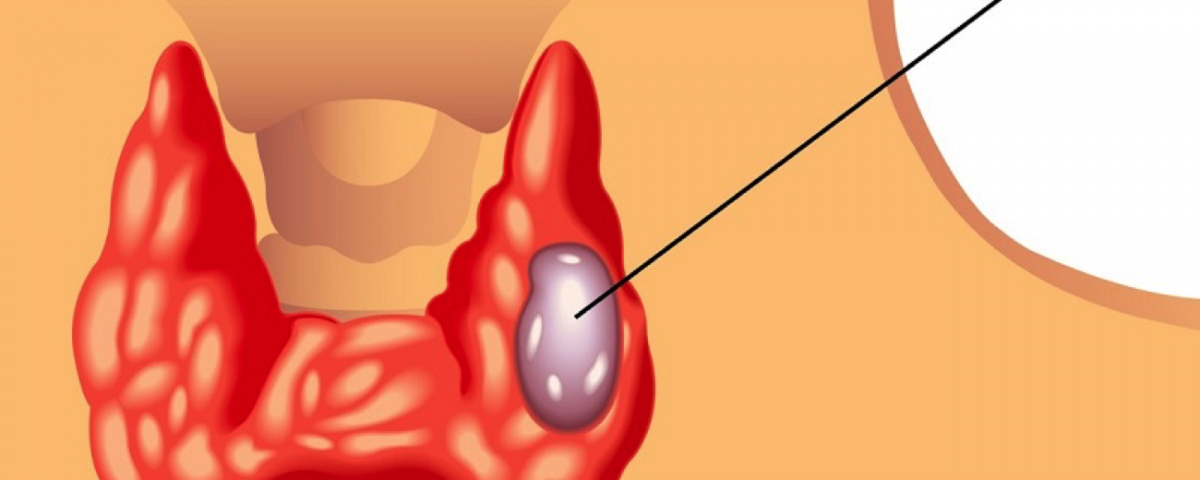
Thyroid cancer is a heterogeneous disease that is classified into differentiated thyroid carcinoma (DTC), anaplastic thyroid carcinoma (ATC) and medullary thyroid carcinoma (MTC). DTC and ATC together are classified as nonmedullary thyroid cancer (NMTC). DTCs are the most common histotype (85%), and include papillary (70%) and follicular (10%–15%) as well as subtypes like Hurthle cell carcinomas. Although activating point mutations of the TSH receptor have been discovered in 60–70% of benign toxic adenomas, a pathogenetic role for these mutations in malignant transformation has been excluded or rarely reported
2. Molecular Target Therapy In Advanced Thyroid Cancer

Recent advances in molecular biology resulted in significant improvement in our understanding of the pathogenesis of thyroid carcinoma
Gene rearrangements involving the RET and TRK proto-oncogenes have been demonstrated as causative events specific for a subset of the papillary histotype. Recently, another oncogene, BRAF, has been specifically associated with PTC with a frequency around 40%. Mutated forms of the H-ras, K-ras, and N-ras oncogenes are found in differentiated thyroid cancer, but the same mutation are also described in benign thyroid lesion.RET-activating point mutations have been found exclusively in medullary thyroid carcinoma (MTC) and these mutations are observed in both sporadic MTC and FMTC.
All the identified mutation on RAS, RET, TRK, and BRAF genes involve MAP kinase activation. An abnormal activation of this pathway is one of the most studied mechanisms of thyroid tumorigenesis. In a lower percentage, other abnormalities have been reported to be involved in thyroid tumorigenesis such as DNA methylation and gene deletions in chromosomes 11q13 and 3p
RAS-activation induces cell division and inhibits cell differentiation. The expression of p21, the RAS-encoded protein, plays an important role in the intracellular signal transduction from the cell surface to the nucleus where it is able to activate genes expression that induces cell proliferation . In thyroid neoplastic cell proliferation RAS role is still poorly known. It has been hypothesized that activated p21 could interact with some thyroid-specific transcription factors such as TTF1 or PAX-8 . RAS activating point mutations have been found in 3 hot spots localized in the codons 12, 13, and 61. RAS oncogene point mutations account for nearly 40% of benign and malignant follicular thyroid tumours while they are rare in the papillary histotype . Interestingly, RAS mutations are more frequent in thyroid tumors of subjects living in countries where iodine intake is inadequate [14].
The RET proto-oncogene is located on chromosome 10q11-2. It encodes for a tyrosine kinase transmembrane receptor involved in the activation of the MAP kinase cascade. The proto-oncogene is normally expressed in a variety of neural cell lineages including thyroid C cells and adrenal medulla but it is not expressed, or it is expressed at very low levels, in normal thyroid follicular cells . RET oncogene activation may be generated either by a fusion rearrangement of the tyrosine kinase domain of RET gene and the 5′ domain of other genes or by activating point mutations . RET/PTC rearrangements have been reported only in PTC and in some cases of benign follicular adenomas [. Activating RET-point mutations have been exclusively found in MTC. Several RET/PTC rearrangements have been described and all of them are characterized by the fusion of the RET tyrosine kinase domain with a housekeeping gene triggering the constitutive RET expression in the follicular cell . RET/PTC rearrangements are related to ionizing radiation exposure which is a well-recognized risk factor for PTC. The evidence of an increasing incidence of RET/PTC rearrangements in childhood post-Chernobyl thyroid carcinomas and the possibility of determining RET/PTC rearrangements in vitro in thyroid cells experimentally exposed to ionizing radiation is a clear proof in favour of a causative connection between radiation exposure and these chromosomal alterations. Despite this evidence, RET/PTC rearrangements have also been reported in unirradiated thyroid lesions . The prevalence of RET/PTC rearrangements in thyroid tumors of patients who had no history of neck irradiation ranges from 2.5 to 35% among different series . The identification of RET/PTC rearrangements in microPTCs suggests that this is an early event in thyroid carcinogenesis On the other hand, RET/PTC positive tumors do not show a tendency of progression to poorly or undifferentiated tumor phenotype . Germline RET point mutations in MTC are mainly localized in the tyrosine kinase domain and in the cysteine domain of the gene.
3. Standard Treatment Of Thyroid Cancer
Radioiodine (131-I) therapy has been used in the treatment of patients with well-differentiated tumors (papillary or follicular). Thyroid cancer tissue has a unique ability to uptake iodine from blood. Like iodine, radioiodine is uptaken and concentrated in thyroid follicular cells by specific membrane transporters. Compared with normal thyroid follicular cells, thyroid cancer cells have reduced expression of the transporter, which may account for the low 131-I uptake in thyroid cancer tissue.
131-I causes acute thyroid-cell death by emission of short path-length (1 to 2 mm) beta rays. 131-I uptake by thyroid tissue can be visualized by gamma radiation scanning. 131-I must be uptaken by thyroid tissue to be effective, resulting in an absence of response in patients whose thyroid cancers do not concentrate iodide, for example, patients with medullary cancer, lymphoma, or anaplastic cancer. Indications for 131-I administration after thyroidectomy in patients with differentiated thyroid cancer include ablation of residual normal thyroid tissue, adjuvant therapy of subclinical micrometastatic disease, and treatment of clinically apparent residual or metastatic thyroid cancer. The efficacy of radioiodine for both scanning and treatment depends upon patient preparation, tumor-specific characteristics, sites of disease, and dose .
4. New Treatment Modalities In Thyroid Cancer
In a near future, Tyrosine Kinase Inhibitors (TKIs) may open a new era in the radioactive iodine refractory DTC and advanced MTC patients treatment. However, the published clinical trials are relatively limited compared to other malignancies and there is only one reported phase III trial in thyroid cancers and many others phase III are ongoing. The difficulty in enrollment of an adequate number of patients to these clinical trials may be a possible reason for this. It may be possible to overcome this difficulty by multi-institutional trials. On the other hand, there is no proof yet that TKIs improve overall survival. Moreover, having a relatively high number of significant undesirable effects, patients must be selected carefully before starting the therapy. Randomised clinical trials for several agents are ongoing.
For More Information-http://thyroidnation.com/thyroid-cancer/